I Had a Ventral Hernia Repair and My Stomach Is Hurting Again
- Example report
- Open Admission
- Published:
Chronic intestinal pain after laparoscopic hernia repair due to mesh graft migration to the cecum: a example report
Patient Prophylactic in Surgery volume thirteen, Article number:37 (2019) Cite this commodity
Abstract
Background
Hernia repair with mesh graft is i of the most common procedures in general surgery. Mesh graft repair is the treatment of choice for umbilical and periumbilical hernias to minimize recurrence. 1 of the rare simply serious complications is mesh graft migration to viscus. These complications can occur months to years after repair and their diagnosis tin exist challenging as they may present as vague abdominal pain merely.
Example presentation
A 74-yr-old gentleman with multiple medical comorbidities was diagnosed with a para-umbilical hernia subsequently which he underwent a laparoscopic hernia repair at our infirmary using a mesh graft with no complications. On postoperative mean solar day ten, he presented to the emergency room (ER) complaining of colicky abdominal pain in the right iliac fossa for i day associated with diarrhea. A Computed Tomography (CT) scan of the abdomen and pelvis showed diffuse wall thickening of the cecum and final ileum with small-scale free air worrisome for perforation. The decision was made in the ER to discharge him home on antibiotics. The patient then returned back multiple times to the ER for the same complaint along with bleeding per rectum for which he underwent further investigations. Months later, the patient presented once again with the same symptoms. A CT scan revealed recurrence of a periumbilical hernia and thickening of the medial wall of the cecum with mesh graft material. The patient was then taken to surgery and intra-operative findings revealed migration of near 50% of the mesh graft size to the cecum and part of the mesh graft was eroding the distal part of ileum just proximal to the ileocecal junction. Adhesolysis and limited right hemicolectomy with ileocolic anastomosis was done. The patient had an uneventful recovery after revisions surgery without any perioperative complications. He was discharged home on postoperative readmission twenty-four hour period 5 and followed upwards at 2 weeks and three months without whatever delayed complications or subjective complaints.
Conclusion
It is important to consider mesh graft migration to viscus as a cause of persistent abdominal pain and haemorrhage per rectum irrespective of the time of presentation post hernia repair.
Groundwork
Mesh graft repair is the handling of selection for umbilical and periumbilical hernias to minimize recurrence [one]. Early complications of hernia repair include wound infection and chronic hurting. Tardily and more serious complications include mesh migration, erosion, sigmoid colon perforation, small bowel obstacle, enterocutaneous fistula and abscess germination [one,2,3].
These complications can occur months to years later the hernia repair [ii]. However, they are rare and it can be difficult to reach the diagnosis [4]. Mesh graft migration could be primary when the mesh graft is not securely attached to the surrounding tissue migrates through areas of least resistance, or secondary mesh graft migration occurs as a effect of foreign trunk reactions that forms granulation tissue and eventually erodes the mesh graft and causes migration through trans-anatomical planes [5, half dozen]. Colonoscopy is the modality of pick for diagnosing mesh migration to the colon, though ultrasound and CT browse can too exist helpful [4]. The migrated mesh graft into the colon can be asymptomatic, mimicking colonic polyp under endoscopy and can even exist invisible on radiological imaging making the diagnosis of mesh migration challenging. Mesh migration to colon mostly presents with lower abdominal pain and tenderness. Other presentations include weight loss, anorexia, intestinal mass, wound site pain with discharge, symptoms of bowel obstruction or asymptomatic presentation [3]. Most common location for mesh graft migration is the urinary bladder. Mesh graft migrating into hollow viscous is rarely seen [4]. Direction of mesh graft migration is past reoperation to remove the migrated mesh graft. Partial bowel resection might be needed in cases of transmigration of mesh graft [seven]. It is vital to ensure that the mesh graft is positioned correctly and sutured to the surrounding fascia to avert mesh graft migration [8]. Hither in we report a case of mesh graft migration to the colon mail umbilical hernia repair in a 74-year-erstwhile male presenting with intestinal hurting and bleeding per rectum.
Case presentation
A 74-twelvemonth-one-time male person, known case of diabetes mellitus (DM), hypertension (HTN), bronchial asthma and hypothyroidism who was diagnosed with para-umbilical hernia. The defect size was 1 × 2 cm, subsequently of which he underwent a laparoscopic hernia repair at our hospital using a fifteen × 20 cm eTPES mesh Bard® Composix™ East/X Mesh (Warwick, RI) with no complications. The patient had uneventful admission period and was discharged home in skillful condition at twenty-four hours ii post-op.
Postoperatively mean solar day x, he presented to the Emergency Room (ER) lament of colicky abdominal hurting in the right iliac fossa for one day associated with diarrhea (v times/twenty-four hours). No other symptoms were reported by the patient. On physical exam, patient had normal vital signs and generalized balmy abdominal tenderness. The maximum tenderness point was at the correct iliac fossa. A Computed Tomography (CT) scan of the belly and pelvis was done which showed diffuse wall thickening of the cecum and final ileum with aberrant configuration of the cecum and ill definition of its anterior wall with minor complimentary air worrisome for perforation (Fig. 1a & b). The decision was made in the ER to discharge him home on antibiotics.
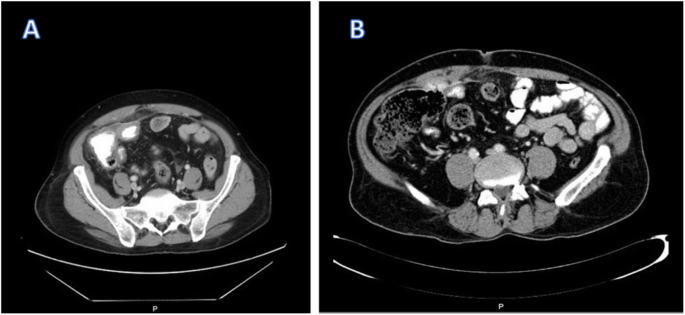
a There is a small free fluid area noted between the bowel loops with possible pocket-sized localized fluid collection seen posterior to the mesh and anterior to the cecum. b Suspicion one mm focal defect inside the inductive cecal wall
10 weeks post-operation, the patient presented once again to his primary surgeon at our establish with the same complains where CT scan was ordered again and showed the aforementioned findings. Colonoscopy was ordered which showed modest polyp that was removed and revealed benign adenoma, also showed a small solid construction in the cecum (Fig. two). Biopsy of that solid structure showed granulating tissues.

Colonoscopy picture showing small solid structure plant in the cecum
Three months after surgery, the patient returned back to his main surgeon lament of haemorrhage per rectum for which he underwent farther investigations including second colonoscopy. The colonoscopy showed a polypoidal mass that was biopsied and showed granulating tissues (Fig. 3). The patient was sent back to the surgeon'southward clinic and reassured.
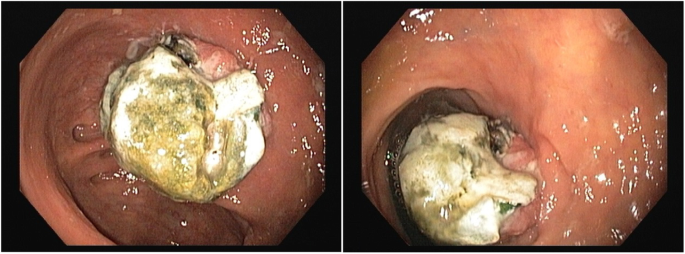
The colonoscopy picture showing polypoidal mass
10 months post operation, the patient was seen in the outpatient dispensary complaining of persistent vague intestinal pain and bleeding per rectum. CT scan of belly and pelvis was repeated which demonstrated opacity at the level of the cecum with dense opacity medial to it of low attenuation and contains some air bubbles (Fig. 4). Some other colonoscopy was done which showed a pocket-sized mass in the cecum (Fig. 5) that was biopsied and revealed to be granulating tissues, the patient was referred to the primary surgeon who reassured the patient and gave him a follow up appointment in one-twelvemonth time.

A mesh graft is noted at the level of the cecum and medial to that a dumbo opacity of almost 7.7 × vi.seven × 4 cm noted, which is medially of low attenuation and contains some air bubbles. (Inflammatory procedure or infectious process at the level of the cecum medial to the mesh)
A colonoscopy showing a small mass in the cecum
Follow up after more than 2 years of surgery indicated iron deficiency anemia and B12 deficiency. Thus, a colonoscopy was scheduled simply the patient could not tolerate the bowel prep. A CT Colonography was ordered which showed a foreign object in the colon, mayhap caused bleeding per rectum where the patient was referred back to the surgeon (Fig. 6a). A CT scan revealed recurrence of a periumbilical hernia and thickening of the medial wall of the cecum with mesh graft material that could suggest a complication of the previous ventral hernia repair with extension of the mesh graft through the cecal wall (Fig. 6b & c). Exploratory laparotomy was offered to the patient only he refused and was discharged against medical communication.
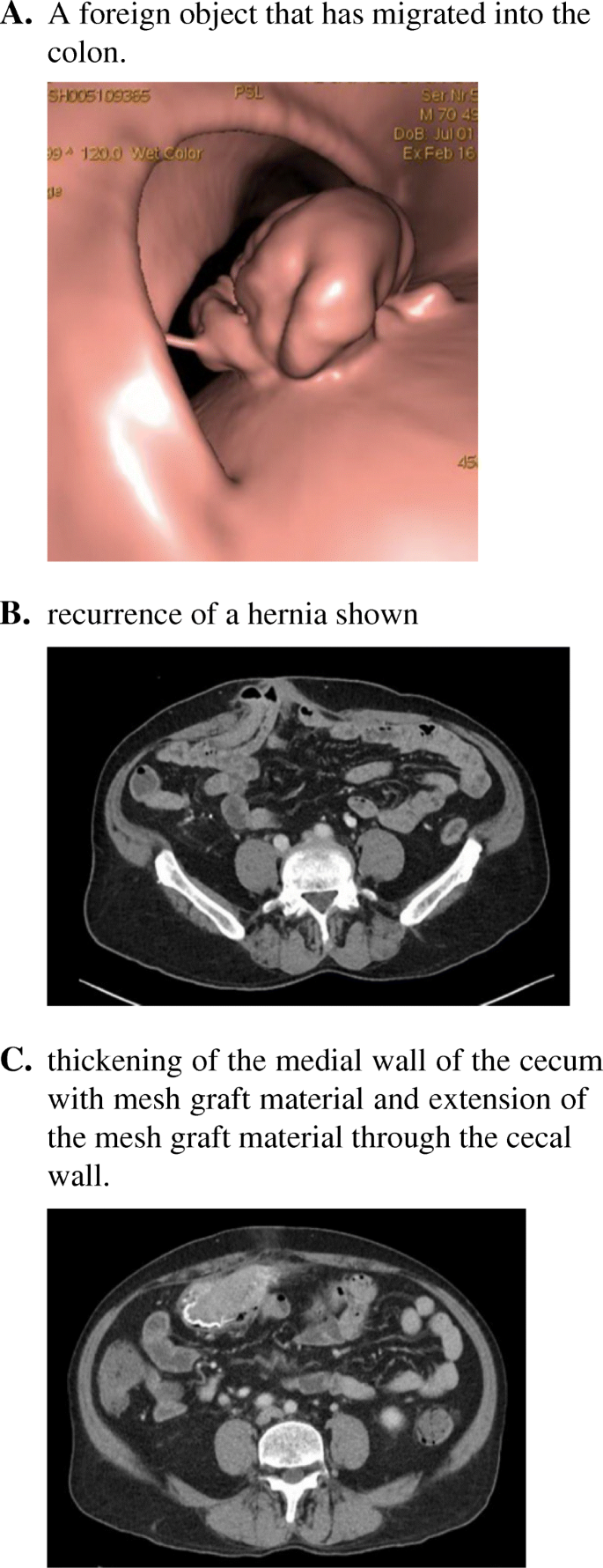
a A foreign object that has migrated into the colon. b recurrence of a hernia shown. c thickening of the medial wall of the cecum with mesh graft material and extension of the mesh graft material through the cecal wall
Ten months later, nosotros received the patient in our service for the offset time when he was complaining of persistent abdominal pain and bleeding per rectum. After reviewing his previous investigations, we told the patient about the mesh graft migration and we discussed with him the mandatory of exploratory laparotomy and mesh graft removal with bowel resection and the possibility of stoma creation at any point of surgery. The patient was informed that he would accept college rate of hernia recurrence and a mesh graft volition not be used in this procedure to avert further complications like wound/mesh infection due to the take a chance of bowel contents spillage in the surgical field on top of his other comorbidities similar DM and bronchial asthma.
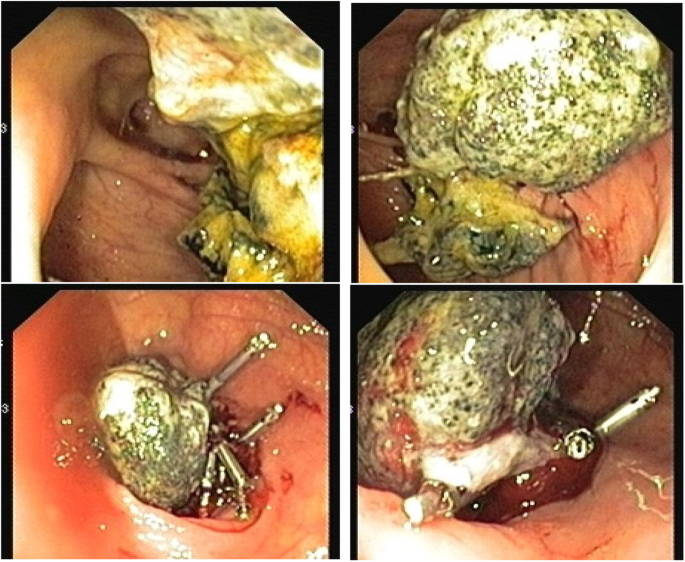
The patient and then was taken to surgery by his principal surgeon, and intra-operative findings revealed migration of almost 50% of the mesh graft size to the cecum and role of the mesh graft was eroding the distal function of ileum merely proximal to the ileocecal junction. Adhesolysis and express right hemicolectomy with ileocolic anastomosis was washed. Fascia closure was obtained primarily without mesh graft application. Skin closure completed with skin clips (Figs. 7, 8 & ix). The patient had an uneventful recovery after revisions surgery without whatsoever perioperative complications. He was discharged home on postoperative readmission day 5 and followed upward at two weeks and three months without any delayed complications or subjective complaints.
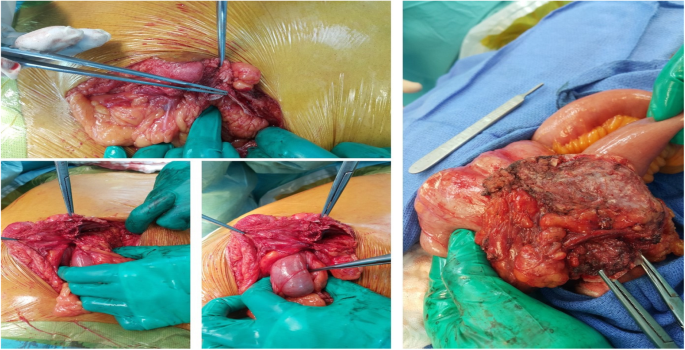
Intraoperative pictures during autopsy of mesh adhesions to small bowel and colon
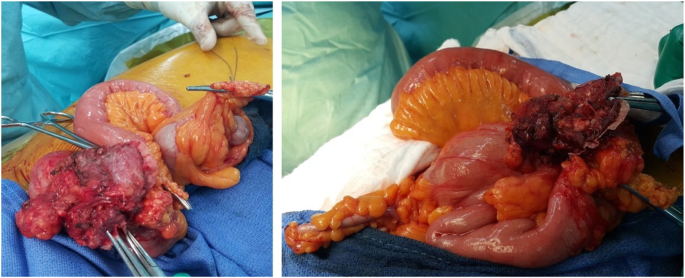
Modest bowel and colon adhesion to mesh graft
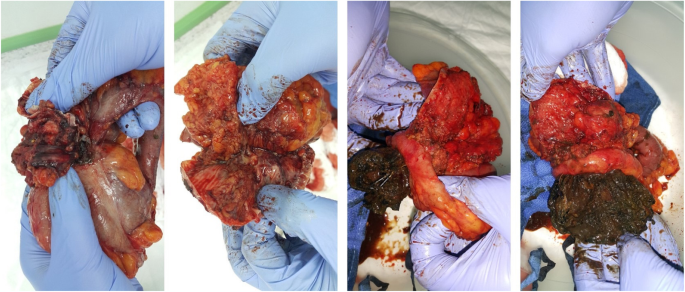
Specimen removed of distal ileum, cecum and proximal office of ascending colon with part of the mesh graft adhesed to the distal ileum bowel and the other office of the mesh graft migrated within the cecum
Discussion
Co-ordinate to the literature, hernia repair with mesh graft is the gilded standard technique for repairing umbilical and periumbilical hernias which helps in reducing the hernia recurrence charge per unit [1]. Due to the nature of the mesh graft being a foreign object, the chance of complications increases later hernia repair such as hematoma, seroma, foreign trunk reaction, organ damage, infection, mesh graft rejection and fistula formation and rarely mesh graft migration [9]. The first reported instance of mesh graft migration was by Herrera et al., in 1976, which migrated into the large bowel 2 years after the repair followed by the second case reported by Majeski et al., in 1998, that migrated and acquired abdominal obstruction 30 years after the repair [1]. Even so, the incidence of mesh graft complications has been reported upwardly to 20%, where meshes migration beingness part of these complications and was recorded at an incident rate of 0.07% [x].
Complications can be classified equally major complications which are life threatening that crave emergency surgery and those that are clinically alarming complications which are meaning but do not require an emergency set-up. Major complications include bowel obstruction, perforation and haemorrhage. Clinically significant complications include enterocutaneous fistula, sinus tract formation, intra-abdominal abscess, seroma and not-healing wound. Complications can also be classified in relation to hernia repair with definite relation or possible relation. Bowel obstruction is 1 such complication which tin be mayhap related to hernia repair if it is correlated with the patient's prior intestinal surgery rather than the mesh graft itself. This can be confirmed past ruling out the presence of adhesion to the mesh graft [3, 9].
Similarly, nigh common long-term mesh graft related complications are bowel obstruction and sinus tract germination, keeping in mind that mesh graft size, which is determined past the size of the hernia, is a take a chance cistron for the development of complications. As well, inflammation related to the mesh graft secures its repair due to fibrosis, compared to loose mesh without fibrosis leading to recurrence of the hernia. Therefore, Multiple measures to reduce the charge per unit of inevitable mesh graft repair complications are considered during the repair [9, 10].
The adventure factors and exact pathophysiology of mesh graft migration is still unknown. However, various factors such as inadequate fixation of the mesh graft to the fascia or sliding due to external forces and entry of the mesh graft into the abdomen from points of least resistance, or presence of adhesions and inflammations from previous surgeries can increase the risk of mesh graft migration. It is too hypothesized that the abrupt edges of the mesh graft can induce an inflammatory reaction which tin can erode the parietal peritoneum and penetrate into the colon [seven]. Mesh graft migration can occur acutely or over a menstruum of years equally a result of inflammation [1]. The surgical technique used, and the surgeon'south technical ability can increase the risk of infection and thereby increment the risk of fistula formation which can somewhen cause mesh graft migration [4]. Additionally, the type of material used in mesh graft construction also determines the rate of infection and the trend of the mesh graft to drift [v]. Interaction of the mesh graft with the surrounding tissue varies depending on the holding of the mesh resulting in different complications associated with different types of mesh graft. Mesh graft erosion and transmigration accept occurred with dissimilar types of mesh graft including polypropylene plug mesh, polyester mesh, Polytetrafluoroethylene (PTFE) and dual layered PTFE and expanded polytetrafluoroethylene (ePTFE) mesh. Though, PTFE is associated with infections, polyester is associated with a chronic foreign torso reaction and polypropylene is associated with an astute inflammatory response somewhen resulting in fibrosis, further studies are needed to compare the incidence of mesh migration in unlike types of mesh graft [7].
On the other hand, in our experience explained above, 1 of the causing factors for such complexity is using large mesh graft 20 × fifteen cm for a small defect especially if information technology was not applied properly which allowed a gap between the mesh graft and the intestinal wall which caused entrapment of the bowel. Likewise, frequent visit of our patient to the emergency with worrisome CT finding brand the diagnostic laparoscopy mandatory and that would salve the patient from undergoing a major surgery similar laparotomy and hemicolectomy.
Patients with mesh graft erosion and migration can present with acute intestinal obstruction, mass formation, bowel perforation and chronic abdominal pain between 1 and 20 years later on repair [three]. The gold standard approach to diagnose mesh graft migration to the colon later hernia repair is colonoscopy [i]. While, ultrasound in the diagnosis of mesh graft migration is helpful, it is limited in most cases. CT, on the other manus, despite its better quality images is also limited in cases of infected mesh that tin result in the germination of inflammatory granulation tissue [3]. In our case, the time to the development of mesh graft migration was four years where the patient presented to the ER several times with intestinal pain. The size of the mesh graft in respect to the size of the hernia in his primary surgery is of nifty concern to the development of his complications and should always exist reflected. CT and colonoscopy were performed for him multiple times and eventually he was diagnosed with mesh graft migration to the cecum. Neglecting early CT scan findings despite their small-scale implications without proper interventions has added to the dilemma of early management to this patient. However, unlike most cases in the literature, there was no formation of fistula and our patient presented only with abdominal pain and bleeding per rectum. Nosotros believe that the crusade of mesh graft migration was due to application of tacker that was prominent to adhere to colon or long infinite between each tacker that allow colon entrapment. Information technology might be prevented by applying trackers as standards and respecting the space between each tacker not to let the colon to entrap or other abdominal structures and also not to forget an important factor which is using the correct size of the mesh for the hernia size. Lastly, shut follow-up to such patients should be of principal objective to achieve desirable outcomes. Our patient was initially managed conservatively for a long menses of time with afar follow-upward appointments and reassurances until the diagnosis of mesh graft migration was confirmed and the recurrence of periumbilical hernia occurred where he underwent a successful surgical repair.
Determination
It is recommended for physicians to exist mindful of the fact that imaging could be misleading towards the diagnosis of mesh graft migration making the diagnosis of mesh graft migration left unnoticed or disregarded. Information technology is important to consider mesh graft migration as a cause of abdominal pain and bleeding per rectum irrespective of the time of presentation post hernia repair. Our case didn't demonstrate a typical presentation like those reported in the literature with fistulas. This case is a reminder that mesh graft migration cases are not always associated with fistulas.
Availability of data and materials
Data sharing is not applicable to this commodity equally no datasets were generated or analyzed during the current report.
References
-
Bostanci O, Idiz UO, Mihmanli One thousand. A rare complication of composite dual mesh: migration and enterocutaneous fistula formation. Case Rep Surg. 2015;2015:293659.
-
Chan RH, Lee KT, Wu CH, Lin WT, Lee JC. Mesh migration into the sigmoid colon mimics a colon tumor, a rare complication afterwards herniorrhaphy: instance written report. Int J Color Dis. 2017;32(1):155–7.
-
Liu S, Zhou XX, Li L, Yu MS, Zhang H, Zhong WX, Ji F. Mesh migration into the sigmoid colon later inguinal hernia repair presenting as a colonic polyp: a case study and review of literature. World J Clin Cases. 2018;half-dozen(12):564–9.
-
Al-Subaie South, Al-Haddad M, Al-Yaqout West, Al-Hajeri Thou, Claus C. A example of a colocutaneous fistula: a rare complexity of mesh migration into the sigmoid colon after open tension-complimentary hernia repair. Int J Surg Case Rep. 2015;xiv:26–ix.
-
Millas SG, Mesar T, Patel RJ. Chronic abdominal hurting afterward ventral hernia due to mesh migration and erosion into the sigmoid colon from a distant site: a instance written report and review of literature. Hernia. 2015;xix(5):849–52.
-
Ceci F, D'Amore Fifty, Annesi E, Bambi L, Grimaldi MR, Gossetti F, Negro P. Chronic anemia due to transmural due east-PTFE anti-adhesive barrier mesh migration in the modest bowel after open incisional hernia repair: a case report. Int J Surg Instance Rep. 2018;53:54–vii.
-
You lot J, Onizuka Due north, Wong L. Transgastric constructed mesh migration, ix years later liver resection. Instance Rep Surg. 2014;2014:412594.
-
Na Y, Sun YH, Sun ZC, Xu HM. Mesh erosion into sigmoid colon after inguinal hernia repair. Chin Med J. 2017;130(ix):1133.
-
Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. Jama. 2016;316(15):1575–82.
-
Oguri Y, Cho H, Yajima K, Oohinata R, Iwasaki Y. Case of complete mesh migration into the stomach after mesh hiatoplasty for a hiatal hernia. Asian J Endosc Surg. 2018;xi(four):395–viii.
Acknowledgements
Not applicable
Annunciation
Authors declare no conflict of interest for reporting this case and the authors do not have any fiscal disharmonize of interest related to any manufacturer or any other industrial entity producing surgical mesh grafts.
Funding
The authors declare that they have no source of funding for this article.
Author information
Affiliations
Contributions
AAlShammari: assistant surgeon, designing and reviewing the article, FAlyousef: literature review and writing manuscript. AAlyousif: literature review and information collection. ZA: literature review and data collection. FAlJishi: literature review and writing manuscript. IS: literature review and writing manuscript. HA: literature review and information collection. MA: surgeon, designing and reviewing the article.
Respective writer
Ideals declarations
Ethics blessing and consent to participate
Ethical approval was obtained by Function of Enquiry Affairs (ORA) at our institute.
Consent for publication
Written informed consent was obtained by the patient for publishing this case and can be sent to editor in chief up on request.
Competing interests
The authors declare that they take no competing interests.
Additional information
Publisher's Notation
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Admission This article is distributed under the terms of the Creative Commons Attribution iv.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in whatsoever medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were fabricated. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the information made bachelor in this commodity, unless otherwise stated.
Reprints and Permissions
Nigh this article
Cite this commodity
AlShammari, A., Alyousef, F., Alyousif, A. et al. Chronic abdominal hurting after laparoscopic hernia repair due to mesh graft migration to the cecum: a instance report. Patient Saf Surg 13, 37 (2019). https://doi.org/10.1186/s13037-019-0220-six
-
Received:
-
Accepted:
-
Published:
-
DOI : https://doi.org/10.1186/s13037-019-0220-6
Keywords
- Hernia repair
- Mesh graft migration
- Cecum
- Abdominal pain
Source: https://pssjournal.biomedcentral.com/articles/10.1186/s13037-019-0220-6
0 Response to "I Had a Ventral Hernia Repair and My Stomach Is Hurting Again"
Post a Comment